
Most of us think that we get fat because we eat too much, however latest scientific research disagrees and suggests that this is too much of a simplistic way of looking at the causes of obesity.
In this article, I explain how the hormone insulin is now thought to be one of the most important contributing factors, I explain the science and how we can use this knowledge to our advantage.
The human body is a wonderfully complex but a logical machine. Everything exists in a fine balance; the body has ways of constantly checking that everything is as it should be, and, if it’s not, it sends signals to intervene to ensure that it returns to baseline.
A new emerging theory about weight gain and obesity is that weight is under the influence of your hormones and conscious control has little influence in managing your weight. Therefore, in order to lose weight you really need to understand what happens when you eat.
The minute you eat food your body gets ready and stands to attention. The smell and sight of food sends signals to your brain asking it to release hormones to help with the digestion and processing of food.
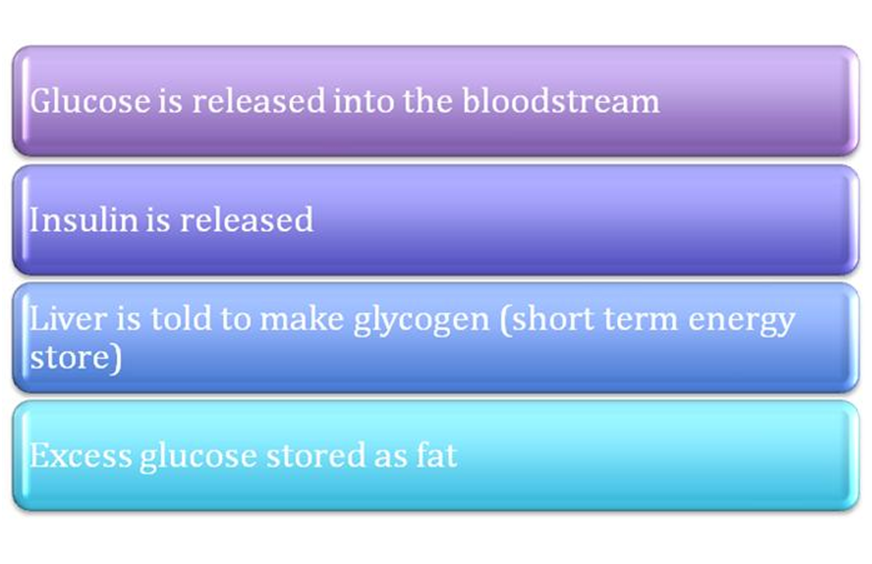
Food enters your stomach, and it mechanically helps with the breakdown of food by contracting and relaxing. Hormones are then released to chemically help with breakdown, as a result glucose levels in our blood go up.
Glucose is the fuel that your body needs to carry out all your functions, but it can’t remain in the blood stream; as a result insulin is then secreted to try and move that glucose to where it can be stored.
Insulin can be thought of as a storage hormone. When it is present in the blood it makes glucose move into cells, so that they get the energy that they need to carry out their essential functions, e.g. breathing, thinking, and moving.
When there is too much glucose, insulin tells the liver to build easily accessible stores of energy called glycogen, in a process called glycogenesis.
The liver does this really efficiently under the control of insulin but has only a limited capacity to store glycogen. So when there is more glucose than the liver can handle, it turns it into fat. This fat is stored in the body either under the skin as subcutaneous fat or around the organs of the body, known as visceral fat. One of the main purposes of fat is to act as a long term energy storage system to be accessed when there is no glucose in the blood for energy and when the liver has used its glycogen store.
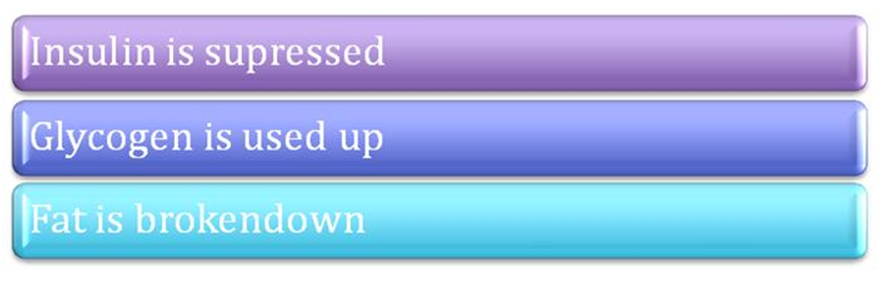
Now let’s look at what happens at the other end. Imagine that it’s first thing in the morning; you last ate food the previous day. You are currently in a ’fasting state’ but, despite this, your body needs energy to perform its essential functions. Obviously there is no food in your system so there is no easily accessible glucose circulating in your blood. Your body then tells your liver that it needs to breakdown the glycogen stores it has saved up to release energy.
As I mentioned earlier, these stores are really limited; when these are used up the body then signals for stored fat to be broken down, in a process known as gluconeogenesis.
Fat is broken down, energy is released, and the body carries on as normal.
Lets recap here, when we eat: During starvation:
During starvation:
Now read that last sentence again:
Fat is broken down, isn’t this what weight loss is all about?
 During starvation:
During starvation: